Sleeping for Two:
Complete Guide to Sleeping While Pregnant
Do you have a future soccer star who loves to practice his moves at 2am? Many prenatal discomforts including back pain, nausea, and fetal movements can result in sleepless nights. Insomnia symptoms include difficulty falling asleep, staying asleep, or waking up too early in the morning.
Fears and anxiety about labor, balancing work, and impending motherhood may also increase the likelihood of developing insomnia.
Pregnancy can be one of the most exciting times in a woman’s life. There is something magical about knowing that a tiny human being is growing inside of you. It is also an incredibly emotional time with joy and anticipation about who your “mini-me” will look like, coupled with worry and fear about whether you are truly ready for parenthood.
I can still remember the excitement I felt when I found out I was pregnant for the first time. After months of coping with the heartbreak of infertility, I was more than happy to endure the morning sickness that confirmed that I was going to be a Mom. Three children (and three pregnancies) later, I can speak from experience when I say that one of the most challenging symptoms that I was not prepared for was the lack of sleep.
There are many changes to a woman’s body during the 9 months of pregnancy, and each trimester brings its own unique challenges that can impact sleep. While a lot of focus is given to “eating for two” during this special time, more and more research is focusing on the underlooked importance of sleeping for two as well. Let’s explore some of the ways sleep is impacted during pregnancy and some tips on how to get more rest.
Body Changes During Pregnancy
There are many physical and psychological reasons why as many as 94% of women face challenges with sleep during pregnancy, according to research published in Obstetric Medicine. Perhaps this is nature’s way of preparing expecting mothers for the many sleepless nights they will face once their little bundle of joy arrives.

While most of these changes are a natural part of the process, understanding how they impact rest can help you to better prepare and cope. (Check out our Map of Pregnancy Sleep below for some ideas on what you can expect in each trimester.)
The American Academy of Sleep Medicine has outlined some of the prenatal side effects that may impact sleep, including:
Hormones
Women experience a roller-coaster ride of hormone changes during pregnancy. Dramatic rises in reproductive hormone levels may be behind some of the disruptions to sleep patterns mothers-to-be face. During the first trimester, estrogen and progesterone steadily increase, peaking at term and rapidly falling after delivery.
Progesterone has been shown to have a sedative effect, explaining why most women experience heightened fatigue during the first trimester when levels of this hormone surge. [1] Both progesterone and estrogen have also been found to decrease rapid eye movement (REM) sleep, the important stage when the brain is consolidating information into long-term memories. (Maybe this explains why so many women “forget” about these challenging symptoms and keep having babies!)
Body Shape
As your little passenger begins to grow and occupy more space, the physical changes that announce your expecting status to the world become noticeable. In the first trimester, most women can keep their pregnancy a secret. Other than thicker hair and that coveted glow mamas-to-be display, most of the changes are happening inside.
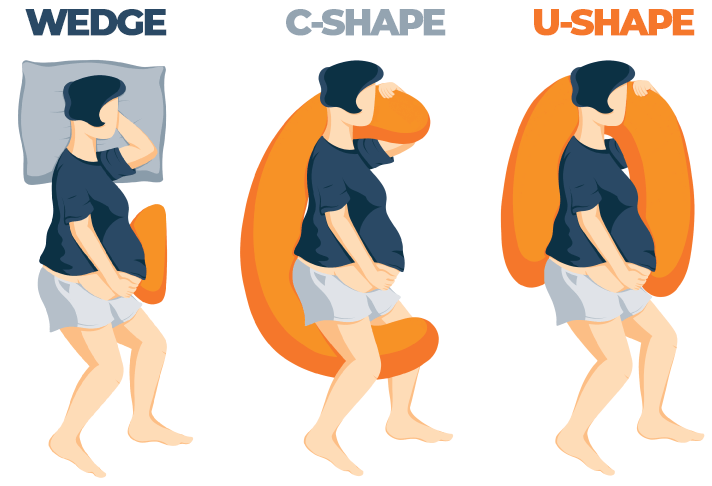
As the first trimester ends, the womb begins to expand to accommodate your tiny seedling’s rapid growth, and many women find that sleeping becomes more of a challenge. Getting into a comfortable position can be difficult, especially for those who are used to sleeping on their stomach or back. This is often the time a pregnancy pillow becomes useful since it can provide support for your growing belly.
Find Out More: Sleeping on Your Back While Pregnant
Appetite
During pregnancy, caloric needs increase by 300-500 calories a day, which explains why you may be so ravenous day and night. While not every expecting Mama craves pickles and ice cream, most do notice an increase in appetite very early on (or about the time when that dreadful morning sickness finally goes away).
Nighttime hours are typically when growth and repair take place in the body, and this could explain why many cravings happen after the sun has set. For some women, hunger pangs are one of the many causes of interrupted sleep. In an online survey of 2,427 expecting mothers, 100% reported frequent nighttime awakenings. While craving a midnight snack isn’t the sole cause of these wakings, it may be a big contributor.
Energy Levels, Increased Fatigue
An increase in progesterone may be why many expecting mothers suddenly find themselves sleeping a lot of the time. This reproductive hormone can leave you feeling very tired and may explain why napping is suddenly your favorite hobby. Energy levels are also decreasing, making it hard to function day-to-day.
Napping can help some women to temporarily increase their energy and make it through until bedtime, but for other women, napping later in the day can make it more difficult to fall asleep that night. Oftentimes, the physical demands of growing a human being are so great that fatigue and lack of energy persist despite extra time in bed.
Increased Urination
Frequent trips to the bathroom are yet another commonly reported symptom mothers-to-be experience. In one study of 270 pregnant women, as many as 77% experienced increased frequency of urination throughout all three trimesters. Nocturia (waking in the night to pee) was also reported by over 75% of women, further contributing to the interruptions in sleep that nearly all pregnant women face.
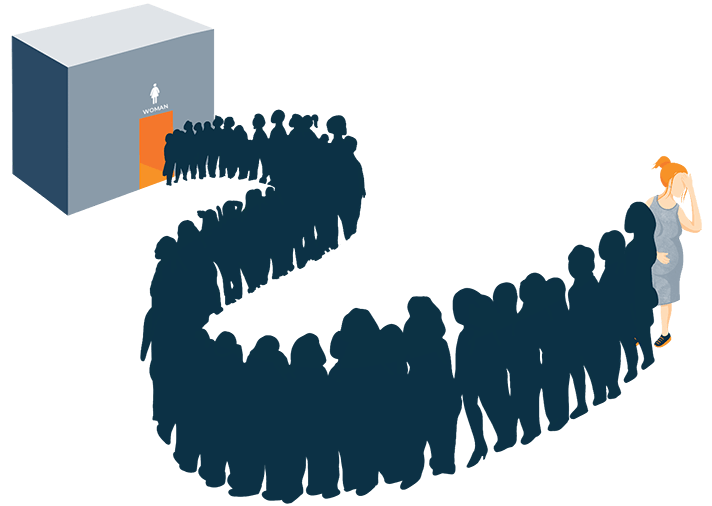
There are many causes for increased urination including rising hormone levels, increased fluid intake, expanding blood vessels, and pressure on the bladder from the growing baby.
Anxiety
- Will my baby be healthy?
- What will labor be like?
- Will life ever be normal again?
These are just some of the many questions that may keep expectant mothers up at night. While some worrying is to be expected during this life-changing season, anxiety that impacts your daily life is not.
Anxiety is an overwhelming response to a perceived threat that is experienced in the body, mind or through behaviors. [2] Some of the signs of anxiety during pregnancy include loss of appetite, irritability, forgetfulness, difficulty sleeping, muscle tension, and trouble concentrating. If you recognize any of these signs in yourself or a loved one, be sure to speak to your health-care provider about treatment options.
Learn More: Anxiety and Sleep
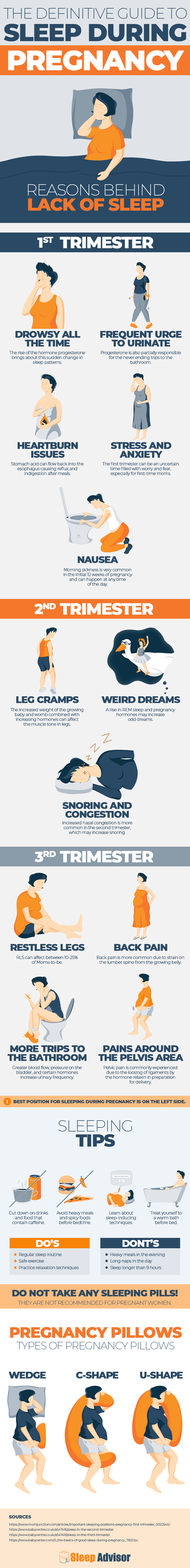
See More: First Trimester Sleep
Why is Sleep During Pregnancy So Important?
Good sleep is one of the most important things an expectant mother can do for her baby. Adequate rest is essential for a healthy pregnancy and full-term delivery.
According to the American Academy of Sleep Medicine, “Not sleeping well can lead to a number of problems. Expectant mothers who have poor nighttime sleep are more likely to have a depressed mood, attention and memory problems, excessive daytime sleepiness, more nighttime falls, and use more over-the-counter or prescription sleep aids, all of which may adversely affect the healthy development of her baby. In addition, recent studies associate lack of sleep with serious health problems such as an increased risk of obesity, cardiovascular disease and diabetes.”
Progesterone Production:
Why it’s Needed
Progesterone is an essential hormone in the reproductive process, playing an important role in fertility and the maintenance of a healthy, full-term pregnancy. Early on, progesterone is produced by the corpus luteum, a temporary endocrine structure in the ovaries. Eventually, the placenta takes over production at around 8-10 weeks.
This hormone is necessary for nurturing a healthy environment for the developing fetus and to prevent rejection by the mother’s body. [3] It also is the reason why you suddenly have luscious locks and that coveted pregnancy glow.
Research has discovered that progesterone activates receptors in the brain that shorten the time it takes for the body to enter REM cycles and also decrease the amount of time spent in this phase [1]. With elevated levels throughout all three trimesters, this hormone may be to blame for your zombie-like state day and night.
Gestational Diabetes
Gestational Diabetes Mellitus (GDM) is a form of diabetes that develops during pregnancy and causes elevated blood sugar levels that the body has a hard time controlling. This is also what doctors are testing for when you have to take that dreaded glucose tolerance test and drink that nasty orange beverage.
Women with (GDM) have an increased risk of developing preeclampsia, are more likely to require a C-section, and are at a greater risk for developing type 2 diabetes after giving birth. Babies born to mothers with GDM have an increased risk of macrosomia, hypoglycemia, jaundice, and birth-related injuries. After birth, these infants are also more likely to develop metabolic syndrome, type 2 diabetes, and obesity later on in life. [4]
In this same study of 686 pregnant women in Asia, shorter durations (< 6 hours per night) and poor quality sleep were independently associated with an increased risk of gestational diabetes. Decreased quality of nighttime rest has been shown to increase hyperglycemia (high blood sugar levels) and insulin resistance, which explains why gestational diabetes is more likely to occur in women who are not getting adequate rest.
Preeclampsia
Many expecting mothers have worried about the risk of developing preeclampsia. This condition is defined as having high blood pressure levels (> 140/90 mmHg) coupled with excess levels of protein in the urine after the 20th week of pregnancy.
Preeclampsia can pose serious threats to both mothers and babies, increasing their risks of serious complications and even death. Both snoring and sleep apnea have been shown to increase the risk of gestational hypertension, which can lead to preeclampsia.
In a cross-sectional study of 311 women, those with preeclampsia experienced more insomnia, snoring, fragmented sleep, and sleep apnea than non-pregnant women. The women with preeclampsia also had higher rates of anxiety and depression than the control groups.
Life After Baby
Many seasoned parents will warn expecting friends to “sleep now while you can.” While fatigue and restless nights can make mothers-to-be long for the days after delivery when they can finally rest in their favorite positions again, sleep after baby can be even more challenging.
Newborns have fragmented sleep patterns in the early days, waking frequently for feedings during the night. Babies who were used to being rocked to sleep by the daily movements of busy mothers may be born with their days and nights reversed. It can take weeks or months for the circadian rhythm to regulate in infants, and nighttime waking can continue into early childhood for some.

Disorders Caused or Made Worse
Christine Won is an MD at Yale and summed up the great irony of sleeping for two in pregnancy when she said, “Herein lies the great paradox of sleep in pregnancy — despite the seemingly imperative need for healthy sleep and our body’s attempt to promote it, many of the normal physiologic and psychological changes accompanying pregnancy make restful sleep all but impossible.” [5]
Unfortunately, many sleep disorders can develop or be made worse during pregnancy, increasing the risk of developing hypertension, gestational diabetes, intrauterine growth restriction, and postpartum depression.
If you suddenly find yourself crying during a toothpaste commercial or snapping at your partner for no reason, you can blame your hormones. Estrogen levels are elevated up to 100 times and progesterone more than 200 times during pregnancy compared to pre-conception levels. [6] These hormone fluctuations coupled with other physical and psychological factors contribute to the higher prevalence of sleep disorders during pregnancy.
Insomnia
Insomnia appears to be a very common struggle that many expecting mothers face with as many as 57% of women reporting this challenge, according to the Sleep Center in Philadelphia. Additional research has found that insomnia may affect women differently depending on which trimester they are in.
Read More: How To Deal With Insomnia After Pregnancy
One study found that “At the beginning of pregnancy, the incidence of insomnia is lower at 12.6% and then increases as pregnancy progresses. Up to 73.5% of women display some degree of insomnia at a median of 39 weeks, further classified as mild in 50.5%, moderate 15.7%, and severe in 3.8%. In the last trimester of pregnancy, up to 69.9% reported difficulty in maintaining sleep, 34.8% described early morning awakenings, and 23.7% reported difficulty falling asleep.”
Restless Leg Syndrome
Have you ever had that creepy-crawly feeling in your legs that you just can’t shake away?
Restless Leg Syndrome (RLS) is a sleep-related disorder that causes irresistible impulses to move your limbs (typically legs). Symptoms tend to be worse in the evening or at night and during prolonged periods of rest.
RLS is twice as likely to occur in females, possibly explaining why it is more common during pregnancy as well.
Gestational RLS prevalence is between 10% and 38% depending on factors like which trimester women are in. [7] Risk factors for gestational RLS include a personal or family history of RLS, a history of growing pains, obesity, smoking, and snoring in the first trimester.
Although it may be tempting to just chalk this up as yet another annoying symptom, RLS can be serious in some cases. A study of 231 women found that there was a two-fold increase in the risk of preterm birth among those with RLS. Preeclampsia is also reported to occur more in women with RLS.
Read More: Best Mattresses for Restless Leg Syndrome
GERD
If you have ever been lying in bed and suddenly felt like a volcano is erupting out of your esophagus, you’re not alone. Gastroesophageal Reflux Disease (GERD) occurs more commonly in women who are expecting with 30-50% reporting frequent heartburn. Pre-existing reflux, increased maternal age, and the amount of weight gained are all risk factors for developing GERD, and the more weight a woman gains, the higher her chances become. [8]
Heartburn, acid reflux, and GERD can all be blamed on those pesky hormone changes that relax the muscles in the esophagus, allowing stomach acids to rise and creating a burning sensation in the throat. As your uterus expands to accommodate your growing baby even more pressure is placed on the stomach, making heartburn and reflux even worse.

Sleep Apnea
Are you suddenly snoring like a log, causing your partner to take cover under his pillow? While some snoring is normal and could be due to more congestion, pauses in your breathing may be worth a trip to the doctor.
Sleep apnea occurs when the upper airways are partially or fully obstructed, decreasing oxygen saturation in the blood and resulting in brief arousals during the night. Although these episodes typically last for only 10-30 seconds, the compound effect they can have on the overall quality of rest is significant.
Several studies have estimated that sleep-disordered breathing during pregnancy occurs in as many as 10-27% of women, with rates increasing with gestational age [7]. Nasal congestion, gestational weight gain, decreased lung volume, swelling or shortening in the esophagus and throat, and large abdominal mass are all contributing factors to the increased prevalence of sleep apnea during pregnancy.
See More: Best Mattresses for Sleep Apnea
Tips For Better Sleeping
Creating a human being is hard work, especially if you are constantly tired and lethargic. Insomnia and fatigue can be challenging to cope with coupled with all of the other prenatal symptoms that can make sleep disturbances worse. Although it may be tempting to reach for an over-the-counter sleep aid or herbal supplement, these are not recommended during pregnancy.
Instead, try these tips which may help to naturally improve the quality of your sleep:
Prioritize Rest
The demands of life will only continue to rise as the day of your baby’s arrival draws closer. Schedule and plan times for rest into your day, even if it just means sitting with your feet up for 5 minutes every hour.
Maintain a Consistent Bedtime/wake-up Time
Get into the routine of going to bed and waking up at the same time every day. This helps to regulate the circadian rhythm and may make it easier to fall asleep quickly at night.
Practice Self-care
Very soon, life will never be the same again. Now is the time to get into the habit of making self-care a priority in your life. Have a pedicure (after all, you probably can’t reach your nails anymore), take a bath, or get a low-maintenance hair make-over (trust me, you will thank me later).
Get Some Exercise
Exercising for at least 30 minutes a day is a great way to improve rest at night. Yoga, walking, and swimming are all great choices, but be sure to check with your health care provider before starting any new exercise routine.
Strategize Naps
Naps can be very rejuvenating when you are battling ongoing fatigue. Try to nap earlier in the day and keep naps to 30 minutes or less to avoid disturbing nighttime rest.
De-stress
Anxiety about your impending delivery and motherhood can keep you up, worrying all night long. Use relaxation techniques to clear your mind like talking to a trusted friend, practicing your faith, journaling, or spending time in nature.
Start Side Sleeping Early
Obstetricians recommend that women sleep on their left side during pregnancy to maximize the flow of blood and nutrients to the baby. Re-conditioning the body to sleep in a new position takes time, so start training yourself to sleep on your side early, before it becomes necessary.
Avoid Big Meals Before Bed
While it may be tempting to give in to late-night cravings, eating large amounts before bed can increase reflux and heartburn. Instead, focus on eating healthy foods earlier on in the day, eating a lighter dinner and a small snack in the evening.
When Should I See My Doctor?
The body is undergoing tremendous changes during pregnancy, and many symptoms like morning sickness and frequent urination are to be expected. However, if you notice that your legs are shaking excessively, you have changes in snoring, your legs and feet are abnormally swollen, or you are experiencing severe headaches, you should speak to your doctor as these could be signs of high blood pressure or other serious complications.
Good Questions for Your OB
What sleeping aids are safe for me?
While most sleeping aids are not approved for use during pregnancy, your doctor may know of over-the-counter or prescription options that have been deemed safe for you.
Is it ok to exercise?
Exercise can be a great way to stay healthy and strengthen your body for delivery. In some cases, exercise may not be safe for all expecting mothers. Speak to your doctor about what types of exercise may be best for you.
What vitamins can help my symptoms?
Growing a baby is hard work for your body, and nutrient needs are at an all-time high. Aside from your daily prenatal, some vitamins can cause harm if taken in large quantities, so always check with your doctor before taking any additional supplements.
Am I sleeping too much?
Getting adequate rest is important for the health of you and your baby. Excessive sleep can be normal in many cases, but if you are worried, speak with your doctor about the number of hours you are sleeping in a day.
What snacks might help me sleep?
Certain foods are high in naturally occurring melatonin, a hormone that helps you sleep. Foods that contain protein and fat are also satiating and may prevent frequent wakings caused by hunger. Your doctor may be able to recommend some good bedtime snack choices as well.
FAQ’s
Is there such thing as sleeping too much during pregnancy?
Several studies have confirmed a link between sleeping in positions other than the left side and an increased risk of still-births, but a recent study also found that excessive sleep (> 9 hours per night) was also associated with a greater number of later-term still-births. While research is still ongoing, you should speak to your doctor if you are concerned about the number of hours you are sleeping and the possible risks for your baby.
Can my sleep predict what kind of labor I’m going to have?
Sleep disturbances in late pregnancy have been associated with delivery type and length of labor. In a study of 131 women in their third trimester, “women who slept





